Harnessing Liver Cell Regeneration: Insights into Mechanisms and Research Applications
The liver has the astonishing ability to regain its original size within days after surgical resection, as demonstrated in rodent studies.
The liver’s natural ability to regenerate has made it easier to treat diseases, including removing tumors by removing part of the organ. Liver cells can restore the liver mass, even after losing 70% of the organ volume. More importantly, the regenerative capacity allows living donor liver transplants, since the liver cells regenerate after partial donation. The main effectors are hepatocytes, while non-parenchymal liver cells orchestrate the process through a complex signal network.
Understanding the cellular mechanisms and contextual factors that shape this regenerative process is key to modeling hepatic regeneration and developing new therapeutic strategies for liver disease.
Cellular and Molecular Mechanisms Driving Liver Cell Regeneration
Hepatic cell regeneration has two main effectors: hepatocytes and biliary epithelial cells (BECs), also known as cholangiocytes.
Under homeostatic conditions, 99% of hepatocytes remain quiescent (G0), with less than 0.2% undergoing DNA synthesis. However, following liver acute injury, liver cells can replace the damaged ones. They rapidly re-enter the cell cycle, supported by the activation of mitogenic pathways involving hepatocyte growth factor (HGF), epidermal growth factor receptor (EGFR), and Wnt/β-catenin signaling. Through hepatic regeneration cell cycle activation, liver architecture is restored.

Figure 1. Factors leading to liver injury. Source: Liu Q et al. Liver regeneration after injury: Mechanisms, cellular interactions and therapeutic innovations. Clin Transl Med. 2024 Aug;14(8):e1812
When hepatocyte proliferation capacity is impaired, it remains controversial which cell is primarily involved in liver regeneration. In chronic liver disease, some researchers support the hypothesis that BECs might play a crucial role (in particular, liver progenitor cells (LPCs) have the capacity to differentiate into hepatocytes and contribute to liver regeneration, albeit at low efficiency. On the other hand, others argue that BECs do not contribute to hepatocyte turnover and are, in fact, the main source of newly generated hepatocytes.
The differentiation of LPCs is tightly regulated by pathways such as Wnt/β-catenin, Notch, and Hippo-YAP/TAZ. While Wnt favors hepatocytic commitment, Notch promotes cholangiocytic differentiation. LPC-driven regeneration is particularly prominent in models of advanced fibrosis or chronic liver disease, where the regenerative capacity of mature cells, mostly hepatocytes but also cholangiocytes, has been exhausted.

Figure 2. Overview of liver regeneration in chronic hepatic diseases. Activation of progenitor cells is induced by senescence or exhaustion of cholangiocytes or hepatocytes. After longstanding hepatocellular damage, macrophages stimulate the proliferation of liver progenitor cells (LPCs) via the Wnt and TWEAK pathway. In chronic cholangiocytic damage, myofibroblasts influence LPCs via the Notch and YAP pathway. In addition, HSC, myofibroblasts, and macrophages regulate the extracellular matrix (ECM) through deposition of collagens and secretion of matrix metalloproteases (MMPs). Source: Van Haele M, Snoeck J, Roskams T. Human Liver Regeneration: An Etiology Dependent Process. Int J Mol Sci. 2019 May 10;20(9):2332.
Non-parenchymal cells, such as Kupffer cells (KCs), hepatic stellate cells (HSCs), and liver sinusoidal endothelial cells (LSECs), also modulate regeneration through inflammatory signaling, matrix remodeling, and angiogenesis. The balance between pro-regenerative and pro-fibrotic signals from these cell types can determine whether regeneration proceeds or fails.
Factors That Influence Liver Regeneration Capacity and Timing
The liver’s regenerative response varies considerably depending on the injury type, severity, and duration. In acute settings, such as drug-induced liver injury, liver cell regeneration is efficient and predominantly hepatocyte-driven. The initiation phase relies heavily on HGF/MET and EGF/EGFR pathways, which converge on downstream effectors like STAT3, ERK1/2, and AKT to trigger hepatocyte proliferation. In contrast, chronic liver injury induces impaired hepatocyte proliferation, a prominent ductular reaction (expansion of reactive BECs and an increase in the number of bile ducts).
Depending on liver zonation, diverse types of hepatocytes are involved in regeneration, although there’s still debate about which ones play the leading role. While some studies suggest pericentral AXIN2+ hepatocytes are more actively involved in renewal, others point to a broader contribution across liver zones, including TERT-high hepatocytes distributed throughout the lobule.
From Injury to Recovery: Non-parenchymal Cellular Responses to Liver Damage
The sequence from injury to regeneration after liver cell damage is orchestrated through dynamic cellular crosstalk:
- After acute injury, hepatocytes upregulate cell cycle genes and initiate clonal expansion. LSECs and HSCs respond to injury by secreting angiogenic and pro-fibrotic signals. Kupffer cells shift from a homeostatic to a phagocytic and immunomodulatory phenotype, clearing necrotic debris and releasing cytokines like IL-6 and IL-33. These cytokines promote the G1/S transition of hepatocytes and facilitate tissue repair.
- Chronic injury is characterized by the accumulation of senescent hepatocytes and BECs, persistent inflammation, and ECM deposition. Activated HSCs contribute to fibrosis through the secretion of collagen and tissue inhibitors of metalloproteinases (TIMPs), and ductular reaction leads to expansion of the biliary compartment. Macrophage polarization is altered, with an increase in pro-inflammatory subsets that further drive tissue remodeling and impede regeneration.
The interplay between cell-intrinsic programs (e.g., senescence, transdifferentiation) and extrinsic signals (e.g., cytokines, matrix composition) defines the trajectory of liver repair. Understanding this balance is essential for developing models that faithfully recapitulate regenerative versus fibrogenic outcomes.
Applications of Liver Cell Regeneration Research
Liver regeneration is not solely a local process driven by hepatocytes and their immediate environment. Recent research from the Spanish National Cancer Research Centre (CNIO) has revealed that liver regeneration is not confined to intrahepatic signaling. Glutamate, released by hepatocytes after acute injury, acts as a systemic signal that activates monocytes in the bone marrow. These then differentiate into macrophages that migrate back to the liver and support tissue repair. This inter-organ communication, described as the glutamate-mediated liver–bone marrow axis, offers a novel perspective on how metabolic and immune pathways converge to promote regeneration.
This mechanism could have therapeutic implications. Glutamate supplementation may represent a non-invasive strategy to enhance liver regeneration in patients recovering from hepatectomy or awaiting transplant. Although these findings stem from animal models, they have been corroborated using bioinformatic analyses on datasets and human hepatocytes.

This reinforces the critical role of experimental systems that incorporate primary human hepatocytes or humanized liver models. Unlike rodent-only systems, these models capture species-specific transcriptional responses and cellular behaviors that are essential for predicting therapeutic outcomes.
As research continues to bridge basic regenerative biology with clinical applications, models based on human liver cells will be indispensable for refining therapeutic strategies, evaluating drug safety, and accelerating the development of interventions that can effectively harness the liver’s regenerative capacity.
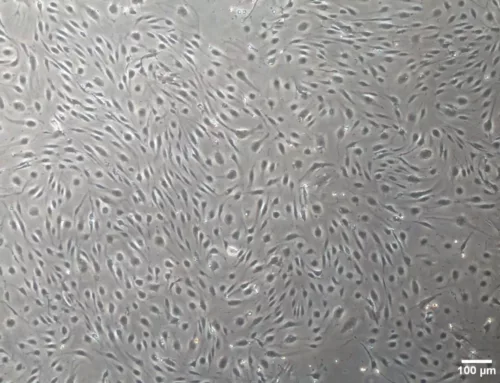
At BeCytes, we are glad to contribute to accelerating research with our primary liver cells.
References
Campana L, Esser H, Huch M, Forbes S. Liver regeneration and inflammation: from fundamental science to clinical applications. Nat Rev Mol Cell Biol. 2021 Sep;22(9):608-624. doi: 10.1038/s41580-021-00373-7.
Liu Q, Wang S, Fu J, Chen Y, Xu J, Wei W, Song H, Zhao X, Wang H. Liver regeneration after injury: Mechanisms, cellular interactions and therapeutic innovations. Clin Transl Med. 2024 Aug;14(8):e1812. doi: 10.1002/ctm2.1812.
Rigual MdM, Angulo-Aguado M, Zagorac S, Álvarez-Díaz R, Benítez-Mondejar M, Yi F, Martínez-Garay C, Santos-de-Frutos K, Kim E, Campos-Olivas R, Djouder N. Macrophages harness hepatocyte glutamate to boost liver regeneration. Nature. 2025. doi:10.1038/s41586-025-08778-6
So J, Kim A, Lee SH, Shin D. Liver progenitor cell-driven liver regeneration. Exp Mol Med. 2020 Aug;52(8):1230-1238. doi: 10.1038/s12276-020-0483-0.
Van Haele M, Snoeck J, Roskams T. Human Liver Regeneration: An Etiology Dependent Process. Int J Mol Sci. 2019 May 10;20(9):2332. doi: 10.3390/ijms20092332.